Comprehensive Lupus Management
Etiology
The exact cause of SLE is not clear, but the interaction between genetic and environmental factors is believed to play a crucial role. Abnormal activation of the immune system leads to autoimmune attacks, resulting in damage to the body's tissues and organs.
Genetic Factors: SLE tends to run in families, and relatives of patients have a significantly higher incidence compared to the general population. The occurrence in identical twins is much higher than in fraternal twins, indicating a relationship between SLE and genetic factors.
Environmental Factors:
Sunlight: SLE patients often experience disease flares after sun exposure, possibly due to ultraviolet-induced cell apoptosis leading to antigen exposure.
Drugs and Chemical Agents: External antigens can activate the immune system, resulting in autoantibody production and tissue damage. Drugs like procainamide, hydralazine, quinidine, and others can induce SLE.
Infections: Pathogenic microorganisms (such as cytomegalovirus, hepatitis C virus, Epstein-Barr virus, etc.) act similarly to drugs, commonly triggering the production of autoantibodies by the immune system.
Estrogen: Most types of SLE are more common in women of childbearing age. Pregnancy and the use of estrogen-containing drugs (such as contraceptives) can exacerbate the disease. Animal experiments have shown that estrogen exacerbates lupus in affected animals, while testosterone alleviates symptoms, suggesting a close correlation between estrogen levels and the onset of SLE.
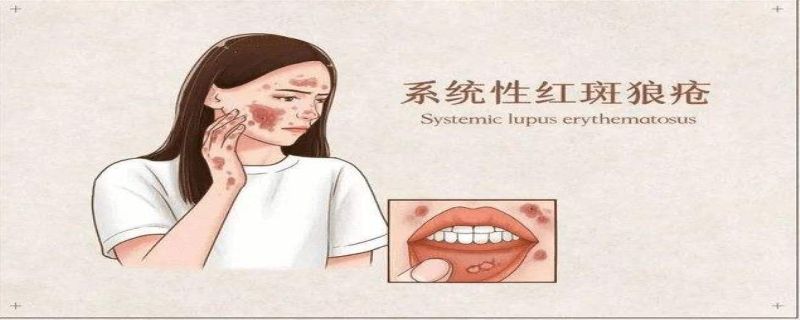
Clinical Manifestations
The clinical manifestations of SLE are diverse and include, but are not limited to:
Skin Symptoms: Rashes, butterfly-shaped facial rash (malar rash), photosensitivity, etc.
Joint Symptoms: Arthritis, joint pain, joint swelling.
Renal Symptoms: Proteinuria, hematuria, which may lead to nephritis.
Cardiac Symptoms: Pericarditis, valvular heart damage.
Central Nervous System Symptoms: Headaches, seizures, cognitive impairment.
Examination
The diagnosis of SLE involves several steps:
Consultation: The doctor inquires about major symptoms, related symptoms, duration, past diagnoses, treatments, family history, etc.
Physical Examination: A comprehensive examination and assessment of the body, including the skin, hair, oral cavity, and joints, among others.
Relevant Tests: Blood tests, urine analysis, imaging studies, kidney biopsies, etc. Kidney biopsies involve a minor surgical procedure where a small piece of kidney tissue is obtained under local anesthesia for pathological and immunopathological examination.
Diagnosis
Apart from typical skin lesions, histopathological examination and blood tests serve as diagnostic evidence. Immunopathological examination is of great value in diagnosis. Positive serum autoantibodies, such as anti-nuclear antibodies (ANA), anti-dsDNA antibodies, anti-Sm antibodies, etc., are characteristic. Changes in antibody titers can reflect disease activity, and active SLE patients often show an increased erythrocyte sedimentation rate. Urinalysis may show proteinuria, red/white blood cells, and cellular casts.