Innovative Brain Recovery Therapies
Causes of the Disease
The sudden acceleration of the head, similar to a sudden blow to the head, can cause brain tissue damage. Rapid impact of the head against an immovable object or sudden deceleration is also a common cause of traumatic brain injury. When brain tissue on the side of impact or in the opposite direction collides with the hard and protruding skull, it is prone to injury. Acceleration-deceleration injuries are sometimes referred to as coup-contrecoup injuries.
Clinical Manifestations
Post-concussion syndrome refers to a condition where a person experiences transient loss of consciousness following a concussion, typically recovering within 30 minutes. Upon regaining consciousness, the patient may not recall the circumstances of the injury or events immediately preceding it. Symptoms may include headache, nausea, dizziness, irritability, emotional instability, lack of confidence, distractibility, and autonomic nervous system symptoms such as pallor, cold sweats, low blood pressure, slow pulse, and shallow breathing.
Coma resulting from traumatic brain injury can vary in duration, ranging from brief to prolonged periods. During the process of recovery from coma to consciousness, patients may experience periods of drowsiness, confusion, and delirium. The level of consciousness fluctuates, with some moments being lighter and others heavier.
Delirium typically arises from a transition out of coma or drowsiness. In some cases, the behavior exhibited during delirium may reflect the patient's previous occupation. Many patients may display resistance, agitation, and non-cooperation, while others may become more aggressive. Symptoms may include terrifying hallucinations, and in severe cases, patients may experience extreme confusion and even exhibit impulsive violent behavior. Delirium can be accompanied by other altered states of consciousness, such as confusion and dream-like states.
Traumatic amnesia syndrome caused by head injury is characterized by fabrication on the basis of forgetfulness, and patients often become easily agitated. Its duration is shorter compared to alcoholic amnestic syndrome.
Subdural hematoma caused by head injury can occur rapidly after the injury, often presenting with headaches and drowsiness. Occasionally, there may be delirious motor excitement, and about half of the patients exhibit papilledema. The characteristics of chronic subdural hematoma include drowsiness, dullness, memory impairment, and in severe cases, comprehensive dementia symptoms. Some patients may have mildly increased cerebrospinal fluid pressure, increased protein quantitation, and a yellow appearance.
Examination
X-ray plain film
Determine fractures, skull sutures separation, intracranial air accumulation, intracranial foreign bodies.
CT Scan
A very important method, which can show the presence and extent of hematomas, contusions, and edema, as well as fractures, pneumocephalus, etc. If necessary, multiple dynamic scans can be performed to track changes in the condition. However, there may be pseudoshadows and poor imaging in the posterior fossa area.
MRI
Although rarely used in the acute phase, it should be considered in cases where lesions in the posterior fossa are poorly visualized on CT. It provides better imaging of intracranial soft tissue structures compared to CT and can be used after the condition stabilizes to assess the extent of injury and estimate prognosis.
Lumbar Puncture
It can measure intracranial pressure and analyze cerebrospinal fluid. When intracranial hemorrhage is accompanied by subarachnoid hemorrhage, lumbar puncture can release bloody cerebrospinal fluid and is also an important therapeutic method.
Cerebral Angiography
Used less frequently in the diagnosis of cranial trauma, but should be promptly utilized when vascular pathology is suspected. In the absence of a CT scanner, it can determine the presence of hematoma based on vascular morphology.
Other Diagnostic Methods
Ultrasound, electroencephalography (EEG), radionuclide imaging, and other methods are of limited significance and are rarely used directly for the diagnosis of cranial and brain injuries.
Diagnosis
Based on the patient's history of injury, along with a thorough examination of the whole body and the nervous system, the diagnosis of cranial trauma can be relatively easily established. The aforementioned examinations can be performed to confirm the diagnosis.
Complications
Brain injuries often result in varying degrees of permanent functional impairments. This largely depends on whether the damage is localized to a specific area of the brain (focal) or widespread (diffuse). Different areas of brain damage can cause different symptoms, aiding doctors in determining the site of injury. Focal symptoms include abnormalities in movement, sensation, speech, vision, and hearing, while diffuse brain damage often affects memory, sleep, or leads to confusion and coma.
Severe brain injuries can sometimes lead to amnesia, where patients cannot recall events before or after losing consciousness, although those who regain consciousness within a week often recover memory. Some brain injuries, even if mild, can result in post-traumatic syndrome, where patients experience headaches and memory impairments for a considerable period.
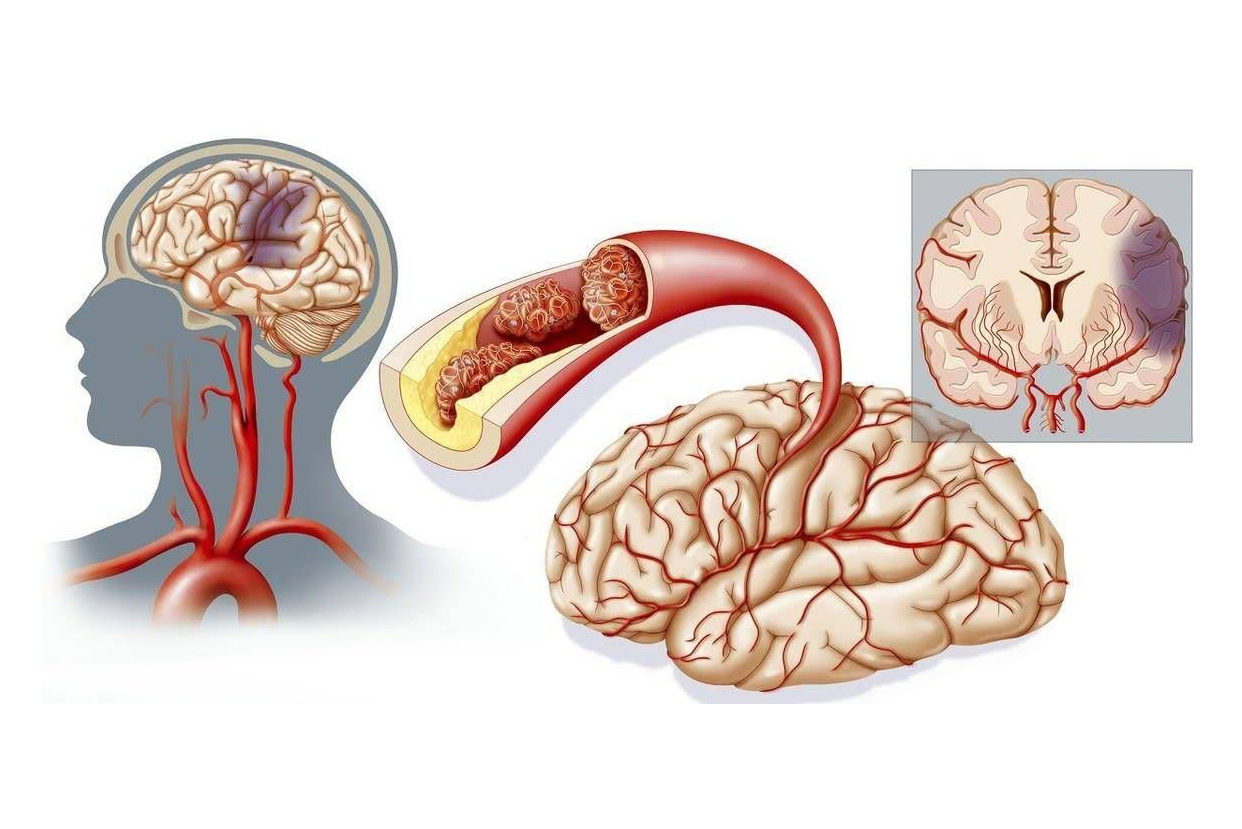
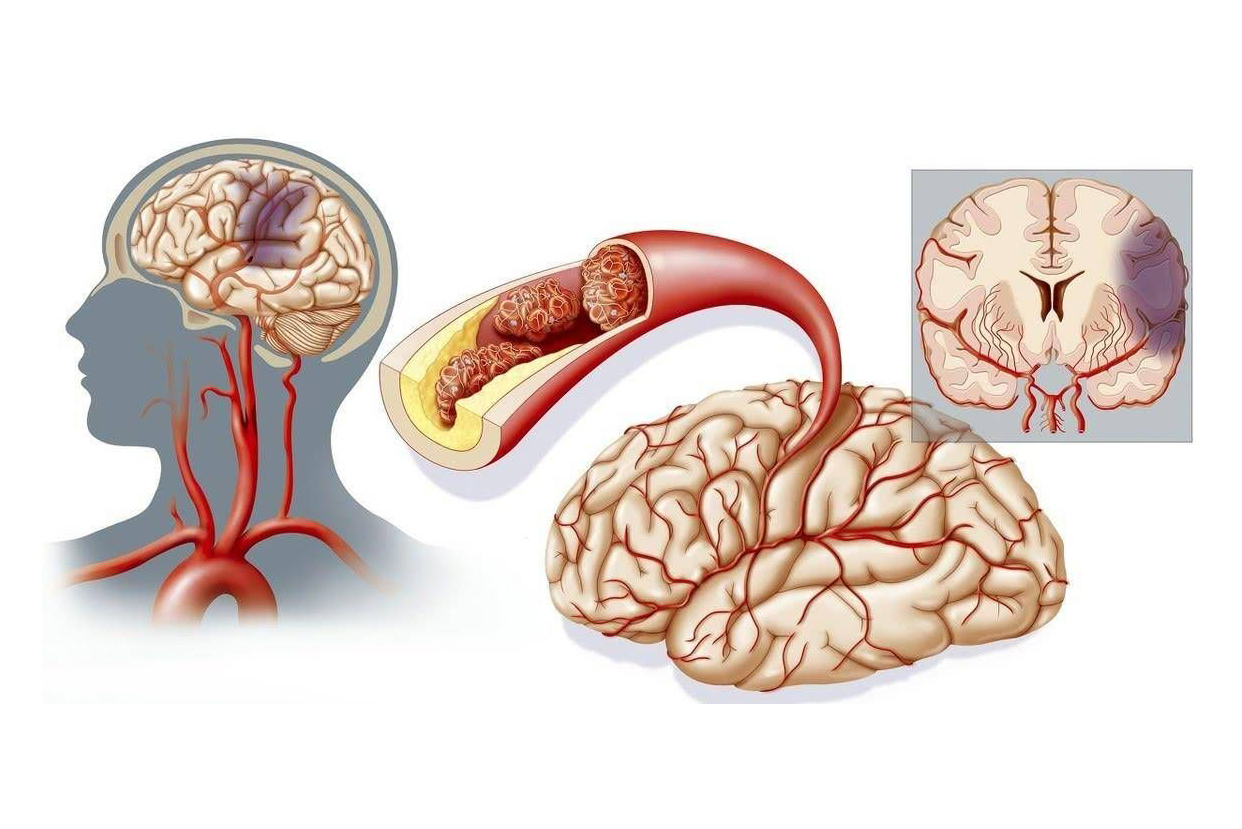
Severe brain injuries can result in stretching, twisting, or tearing of nerves, blood vessels, and other tissues within the brain. Damage to neural pathways or bleeding and swelling can occur. Intracranial bleeding and brain swelling cause an increase in the volume of intracranial contents, but the skull itself cannot expand accordingly. As a result, intracranial pressure rises, further damaging brain tissue. Increased intracranial pressure pushes the brain downward, forcing upper brain tissue and the brainstem into associated openings. This situation is referred to as brain herniation. The cerebellum and brainstem can displace through openings at the base of the skull. Since the brainstem plays a crucial role in maintaining respiration and heart rate, brain herniation can often be fatal.